A research team at the University of California, San Francisco (UCSF) has published early results from a large-scale COVID-19 study, TemPredict, revealing that the Oura Ring temperature sensor could be an effective tool for fever monitoring and early illness detection.
Oura’s CEO, Harpreet Singh Rai, shares his thoughts “Every year, around cold and flu season, users reach out to us saying that Oura caught their fever or let them know that they were about to get sick. We hear often that users see their Readiness Score fall before they feel symptoms of being ill. The initial data from the TemPredict results are showing the same phenomenon. Data in this study suggests that Oura Ring can see changes in data 76% of the time before users feel symptoms of COVID-19. According to the CDC, you can be infectious with COVID 2-3 days before you’re aware of symptoms. If we can catch signals in that window, we can make a difference early and we can help stop the spread. We see tremendous value for every Oura user but also for organizations such as our partners like the NBA and others to help them manage COVID-19 and every flu season.”
—
In our new COVID-19 reality, at restaurants, schools, and public venues, we are becoming accustomed to frequent “temperature checks.” Devices are pointed at our foreheads to measure whether our temperature is above 38°C/100°F to determine whether or not we have a fever. However, this UCSF research highlights the many ways in which this method falls short at doing just that by:
- Relying on Limited Data: When compared to continuous temperature data, measuring temperature at a single point in time provides limited information for accurately identifying a fever.
- Relying on Population Benchmarks: Using single values for classifying fevers (e.g., considering any temperature above 38°C/100°F a fever) doesn’t account for the natural variation in individual temperature across the human population.
- Treating Skin and Core Temperature as Synonymous: Core and skin temperature are two distinct yet coordinated parts of your body’s temperature system. While your core temperature is typically estimated with an oral thermometer, skin temperature can be measured from many places on your body, including your forehead or finger. Though your body aims to hold your core temperature constant (and therefore only yields small variations in a day, ~1-2°C/2-4°F), your skin temperature captures the full physiological range of your body’s temperature changes and can vary by ~15°C/27°F or more in a day. As a result, skin temperature reveals complex temperature patterns which can be parsed for signs of fever or impending illness. However, with more fluctuations comes the need for a more personalized context to identify what is “normal” or “fever-like” for you.
In light of these shortcomings, the researchers establish the potential of using devices like the Oura Ring to improve fever detection and early illness prediction by enabling us to:
- Make Data-Driven Decisions: Oura collects temperature data continuously rather than sporadically, providing 1,440 daily data points rather than single measurements.
- Create Personalized Benchmarks: Oura establishes personalized temperature ranges, which may prove crucial for individualized fever and illness detection.
- Leverage Skin Temperature Patterns: Oura captures meaningful patterns in skin temperature variation directly from your finger rather than being limited to the restricted range of core temperature.
- Spot Multiple Signs Of illness: In addition to temperature, Oura captures changes in resting heart rate, heart rate variability (HRV), and respiratory rate that show early illness detection potential.
Oura’s potential to monitor fever and early signs of illness could eventually enable large-scale health-monitoring research and provide high-temporal resolution data on fever responses across diverse populations.
Want the detailed findings? Read on.
What Data Was Analyzed?
Although TemPredict now has over 65,000+ participants, these initial results focus on the first 50 who reported COVID-19 infections. This smaller sample enabled the researchers to rapidly share proof-of-concept findings, in advance of their final report, for using the Oura Ring as a widely and commercially-available fever monitoring tool.
The dataset contains Oura Ring standard metrics as well as additional research-enabled temperature data sampled throughout the day.* The researchers additionally paired Oura data with daily self-reported symptom questionnaires from UCSF.
Why Oura?
Oura sets itself apart from other wearables by measuring skin temperature directly from your finger and collecting research-grade temperature data every minute. The ring form factor also makes it uniquely comfortable to wear while sleeping, ensuring that temperature data is collected effectively throughout the night—a key time period where the immune system is activated and temperature can reveal valuable information about an individual’s health.
You can read more about Oura’s temperature capabilities here:
- Oura’s Temperature Sensor Validation
- Why Oura Measures Skin Temperature And Not Core
- How Your Temperature Fluctuates Daily
What Did They Find?
While the full report can be accessed here (published in Nature’s Scientific Reports), below are some of the key findings:
- Current fever detection methods lack personalization
- Personalized data could help spot signs of fever
- Fever patterns could be identified even before symptoms are reported
- Continuous skin temperature warrants further investigation for predictive patterns for fever & illness
Current Fever Detection Methods Lack Personalization
In this paper, the researchers highlight how current temperature measurement methods (e.g., scanning your forehead or using an oral thermometer) are insufficiently personalized to capture fevers in the face of the natural temperature variation in the human population.
They note that current methods are ill-equipped because they rely on:
- Measuring temperature at single time points: “Individual and government efforts to track the spread of SARS-CoV2…have employed thermometry at largely random timepoints, for example when entering a workplace or boarding a bus. However, single-point measures have limited sensitivity to detect disease, particularly in the earliest stages of onset.”
- Relying on single values as fever cutoffs: Lacking crucial individual context, these population benchmarks (i.e., 38°C/100°F) fail to capture complex daily patterns in our individual temperatures that are caused by “temperature-modulating biological rhythms” such as circadian rhythms or hormone phases like the menstrual cycle. As a result, “inferring fever from a single-thermometry assessment is reliable only when the fever is well outside the range of these normal variations.”
The researchers underscore the need for personalized temperature data by sharing the substantial variability among TemPredict participants, both in their average temperatures and temperature ranges throughout their healthy baseline and while reporting COVID-19.
In the annotated images below, a line demonstrates how a population-level fever benchmark can misidentify fever in individuals with a higher natural temperature range or miss a fever in individuals with a lower natural temperature range.

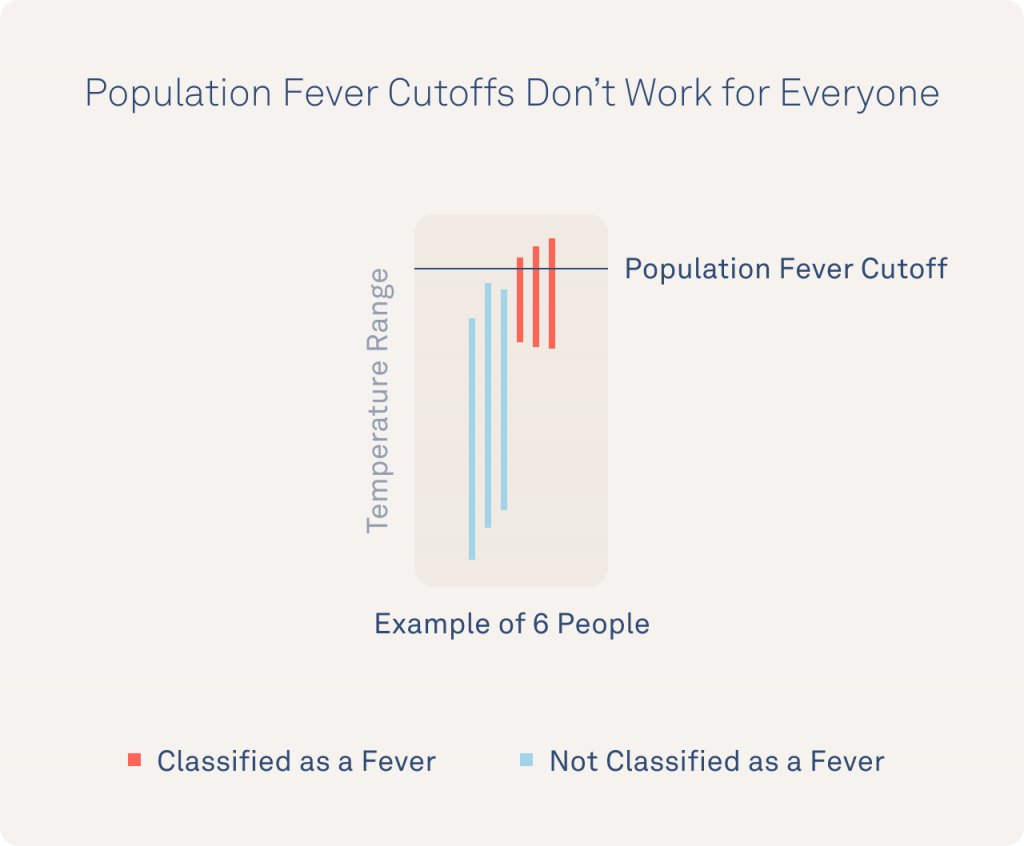
This data highlights just how important personalized context is for identifying fevers (i.e., an abnormal temperature elevation) vs. an individual’s true “normal” temperature. This research illustrates the value of Oura and its ability to provide both continuous temperature data (to capture the full range of an individual’s temperature) and personalized baselines (to individualize insights rather than rely on population benchmarks).
Personalized Data Could Help Spot Signs of Fever
Although the researchers concluded that population benchmark fever cutoffs don’t work for everyone—they proposed a solution. Analyzing an individual’s daily temperature data can reveal patterns that might enable fever detection.
The researchers highlight how observing an individual’s typical temperature rhythms can help spot if they are cycling through their normal patterns or are showing signs of disruption that may indicate strain or fever. More specifically, they highlight how identifying disruptions in an individual’s minimum and maximum average temperature over the course of a day can sound the alarm for a potential fever.
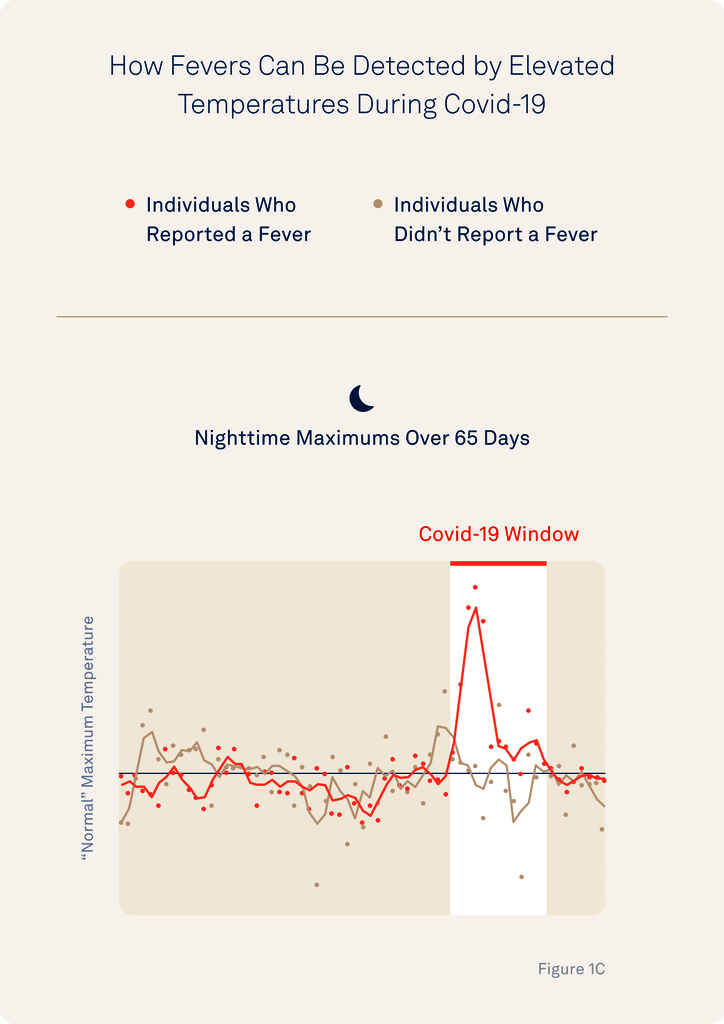
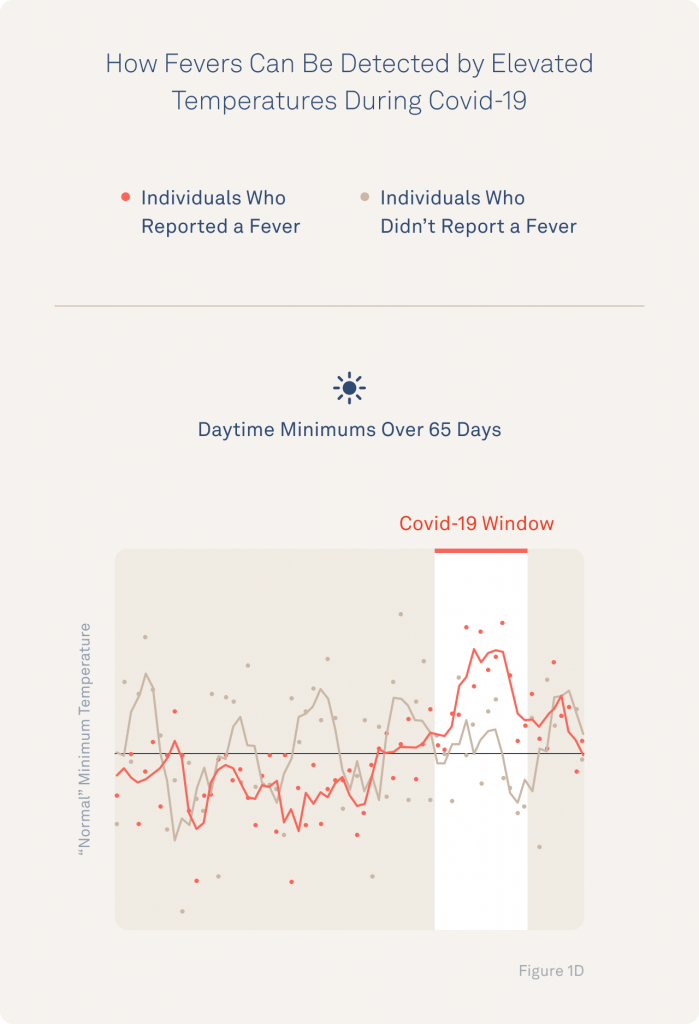
These findings underscore the importance of having sufficient, continuous long-term data to get a clear picture of an individual’s normal temperature rhythms. Oura’s advantage is its ability to sample data every minute, providing 1,440 potential data points in a single day for the sophisticated temperature modeling that could eventually enable personalized fever detection.
Fever Patterns Could Be Identified Even Before Symptoms Are Reported
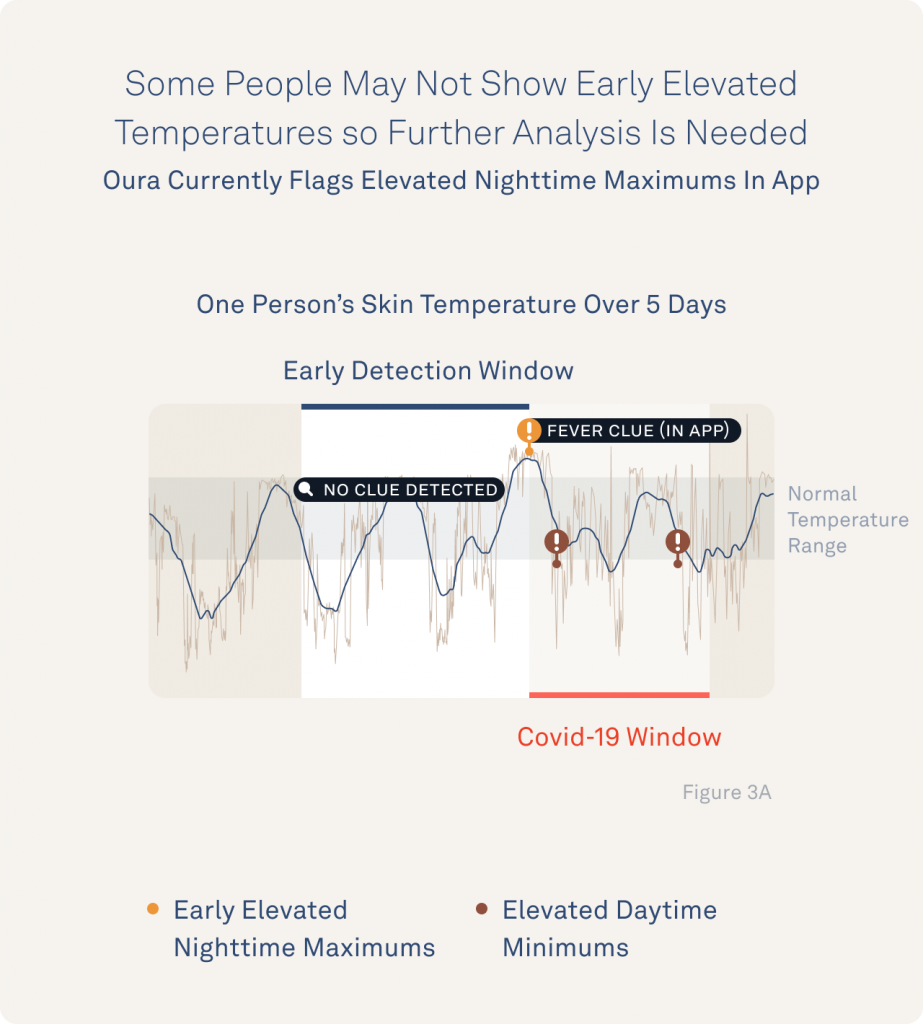
Additionally, in those participants whose patterns displayed disrupted minimum and maximum temperatures, the researchers found encouraging evidence that fever signs could even be spotted in advance of them experiencing fever symptoms. For example, the researchers share how minimum daily temperatures show signs of disruption a few days in advance of symptoms.
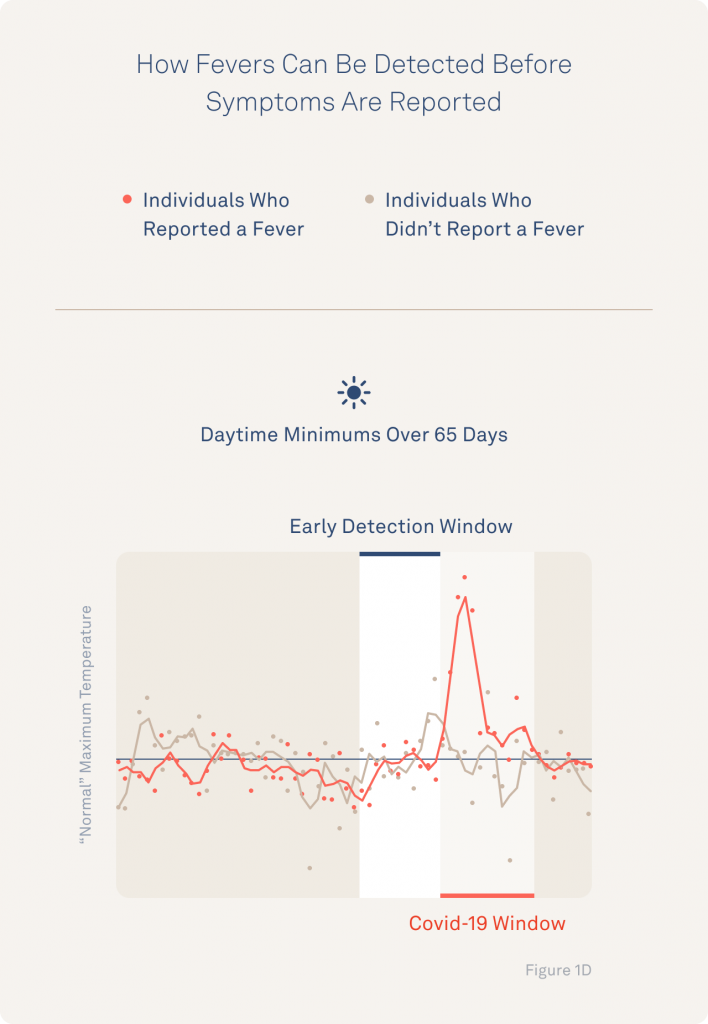
Exactly which patterns are meaningful and useful to each person would still need to be explored before a reliable fever detection tool could be developed—but the implications are promising.
They highlight these findings with a representative example of an individual whose minimum and maximum temperatures are clearly elevated several days before the participant reports their first fever.
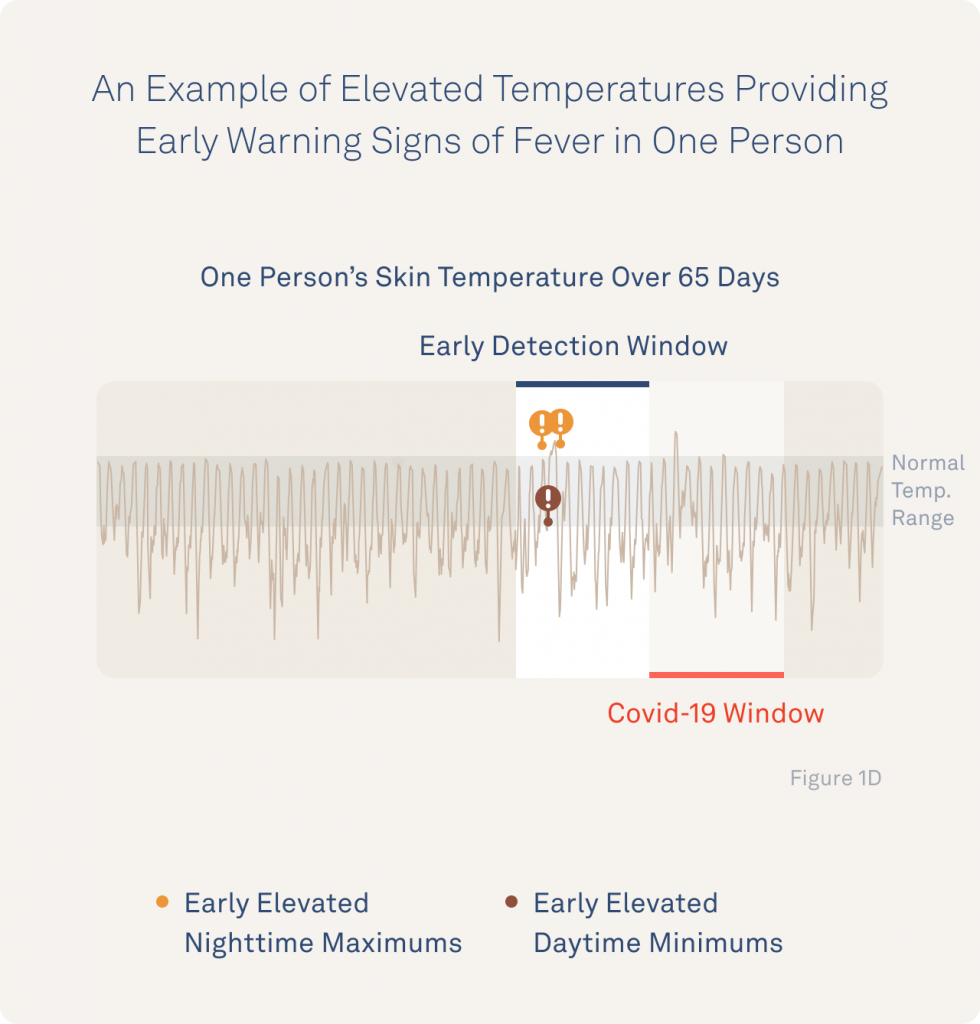
Although Oura’s consumer app currently focuses on nighttime temperature values, these initial findings highlight the benefits of having research-grade temperature data available from the Oura Ring during the day as well.
Continuous Skin Temperature Warrants Further Investigation for Novel Biomarkers of Fever & Illness
The researchers confirm skin temperature’s value for both capturing a wide range of temperature variations throughout the day and for revealing signs of disruption during fever and illness.
So, why does skin temperature capture more temperature variation than core?
Well, your body holds your core temperature as constant as possible, within a narrow range, by sending heat to and from your extremities. This means that measuring temperature changes at measurement sites that estimate your core temperature (like your mouth) will only yield small daily variations, ~1-2°C/2-4°F. By contrast, your skin temperature changes ~15°C (27°F) or more throughout the day and therefore captures the smaller temperature fluctuations that happen minute to minute and hour to hour. These fluctuations are not just “noise” (or the result of washing your hands in cold water) but a valuable window into the natural rhythms of your body. Research suggests that they reflect rhythms encoded within your brain that impact hormone activity and regulate your immune system, metabolism, and cardiovascular health.
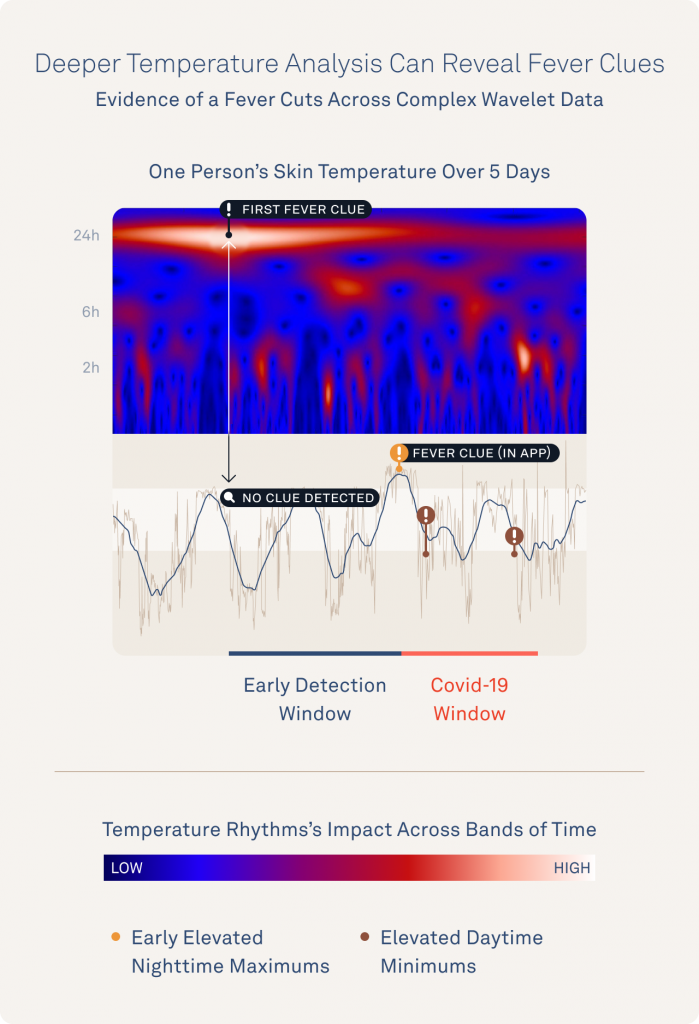
As a result, even hourly temperature rhythms can be parsed for fever and illness detection “clues” by identifying when an individual’s patterns look normal vs. when those norms appear disrupted.
The graphic below shows signs of disruption that the researchers have already discovered during fever and illness. This image shows how analyzing daily temperature pattern changes even within individual days might unearth meaningful information about an individual’s fever or illness risk.
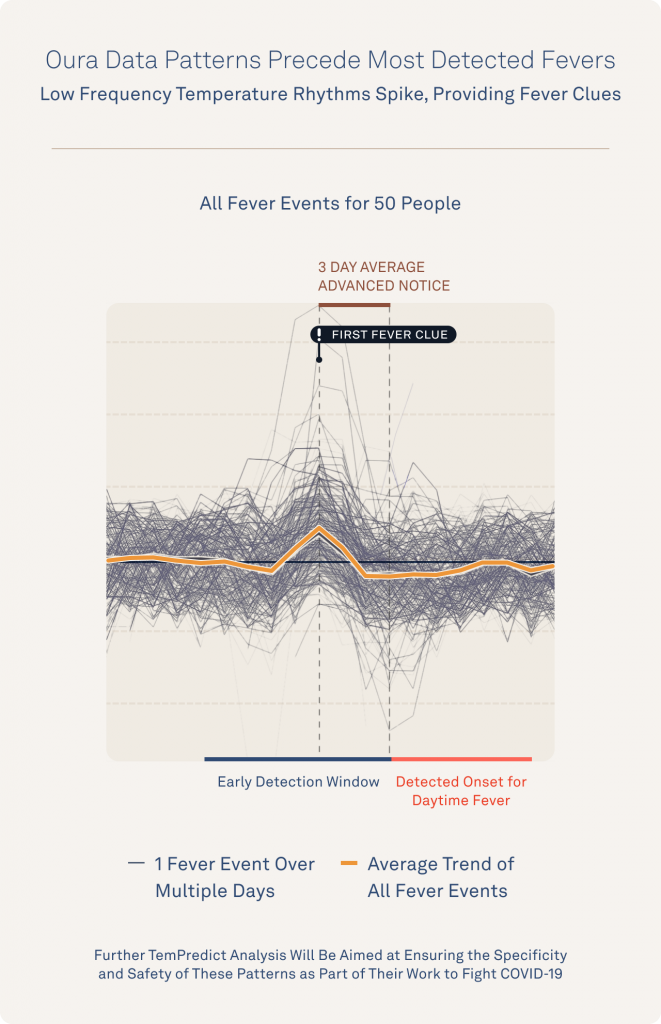
You can see this same “first fever clue” pattern echoed across a graphic of every fever example from these first 50 TemPredict participants.
What’s Next?
The power of personalized temperature measurements in wearables like the Oura Ring is still significantly untapped. But, before the TemPredict study, there wasn’t any compelling research that showed the potential of leveraging skin temperature to detect and monitor illness or fever.
Now there is, and as the novel value of continuous skin temperature monitoring becomes clearer, and temperature continues to play an important role in our lives, we will continue highlighting research that has the potential to make a difference.
Traditional thermometers may be helpful tools but wearables like Oura have the potential to capture personalized patterns and detailed rhythms that those traditional tools cannot, even while we’re sleeping.
While a thermometer can be a helpful temperature measurement tool now, Oura hopes to bring temperature monitoring and illness detection into the future by bringing individuals back into the conversation surrounding our health.
*Note that the Oura App displays only nighttime temperature data, and none of the fever detection or illness findings within this research are currently developed features.